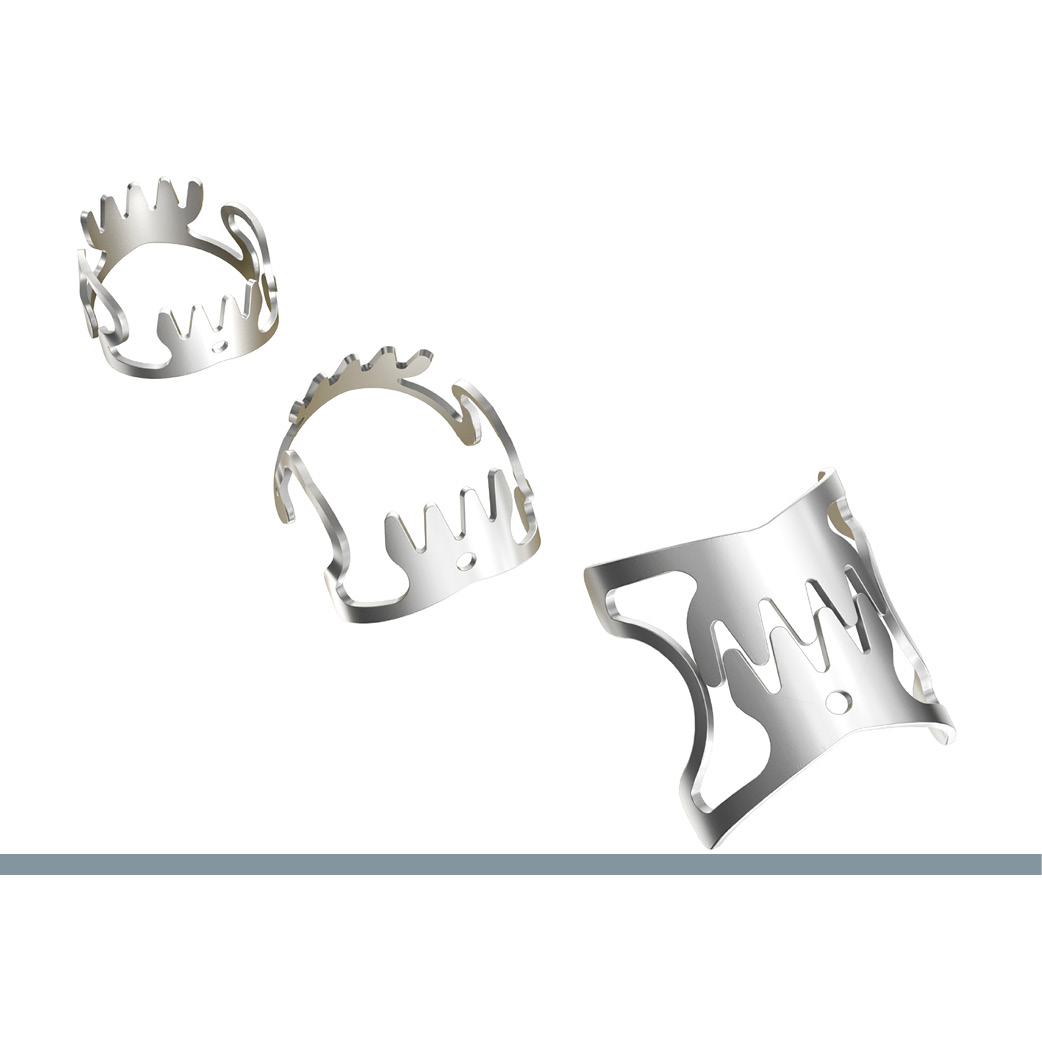
Largest multicenter RCT on OTSC®
Largest multicenter RCT on OTSC® shows superiority to standard hemostatic therapy and confirms first-line treatment for non-variceal high-risk lesions
In patients with non-variceal upper gastrointestinal bleeding OTSC revealed a significantly lower risk for further bleeding than standard endoscopic hemostatic treatment (3.2 % vs 14.6 %; p = 0.006).
Lau et al., Department of Surgery, Prince of Wales Hospital, the Chinese University of Hong Kong, Hong Kong, China, conducted a multicenter randomized controlled trial (RCT) to compare the OTSC System to standard endoscopic treatment in patients with active bleeding or a nonbleeding visible vessel from a nonvariceal cause on upper gastrointestinal endoscopy. Overall, 190 adult patients were included in the trial between January 2018 and December 2020 and randomly assigned at a 1:1 ratio to receive OTSC (n = 93) or standard treatments (n = 97). Primary treatment in the standard group was combined epinephrine injection and thermocoagulation or hemoclips. Endoscopic criteria for randomization were active bleeding (Forrest Ia or Ib) or a nonbleeding visible vessel (Forrest IIa or IIb if vessel unveiled after clot removal).
Primary outcome was the probability of further bleeding defined by the composite of failure to control bleeding after assigned endoscopic treatment and recurrent bleeding within 30 days. Secondary outcomes included failure to control bleeding with assigned endoscopic treatment, recurrent bleeding after initial hemostasis, further intervention, blood transfusion, hospitalization, and deaths from all causes within 30 days. Baseline characteristics of the patients were comparable in the OTSC and standard group, with a mean age of 62.4 vs 64.1 years and most male patients (about 80 %). Mean Glasgow Blatchford score was 10.9 and 11.0, respectively. 29.0 % of patients in the OTSC arm and 35.0 % in the standard arm were on anticoagulation or platelet aggregation inhibition. In both groups most bleedings occurred from a peptic ulcer (92.5 % and 89.7 %). Analysis was done by intention-to-treat.
The cumulative probability in 30-day further bleeding was 3.2 % (3 of 93) in the OTSC group and 14.6 % (14 of 97) in the standard treatment group (risk difference, 11.4 percentage points [95 % CI, 3.3 to 20.0 percentage points]). Failure to control bleeding at index endoscopy was 1.1 % (1 of 93) vs. 6.2 % (6 of 97) (risk difference, 5.1 percentage points [CI, 0.7 to 11.8 percentage points]). Recurrent bleeding after endoscopic hemostasis was also lower in the OTSC group (2.2 % (2 of 93) vs. 8.8 % (8 of 97); risk difference, 6.6 percentage points [CI, -0.3 to 14.4 percentage points]). In peptic ulcers ≥ 10 mm in size, OTSC reduced the rate of further bleeding in comparison to standard therapy (1 of 48 vs. 8 of 46). Red blood cell transfusion, the 30-day intervention for recurrent bleeding and death did not differ significantly between the two groups. There were two device-related serious adverse events in the OTSC group. A patient developed pyloric obstruction after OTSC treatment of a small antral ulcer. The OTSC was cut using a remOVE DC Cutter. A 96-year-old woman was found to have pneumoperitoneum from an ulcer perforation. She declined surgery and died on day 8. Lau et al. assessed the role of OTSC as unclear in this case since endoscopy with gas insufflation alone could have opened up a sealed perforation.
The authors concluded that OTSC treatment is superior to standard endoscopic treatment when used as first-line hemostatic therapy for high-risk non-variceal lesions.
Comparison of Over-the-Scope Clips to Standard Endoscopic Treatment as the Initial Treatment in Patients With Bleeding From a Nonvariceal Upper Gastrointestinal Cause : A Randomized Controlled Trial.
Lau JYW, Li R, Tan CH, Sun XJ, Song HJ, Li L, Ji F, Wang BJ, Shi DT, Leung WK, Hartley I, Moss A, Yu KYY, Suen BY, Li P, Chan FKL.
Ann Intern Med. 2023 Mar 7. Epub ahead of print.
DOI: 10.7326/M22-1783
 |


 Deutsch
Deutsch  Français
Français