In 96 patients with complex anorectal fistulas, OTSC Proctology application lead to an overall healing rate of 65 % and a success rate of 79 % for first-line fistula therapy.
Prosst RL, Proctological Institute Stuttgart, Germany, and Joos AK, Center for Rectal and Colonic Diseases Mannheim, Germany, published follow-up data on 96 consecutive patients who underwent treatment of complex anorectal fistulas with the OTSC Proctology.
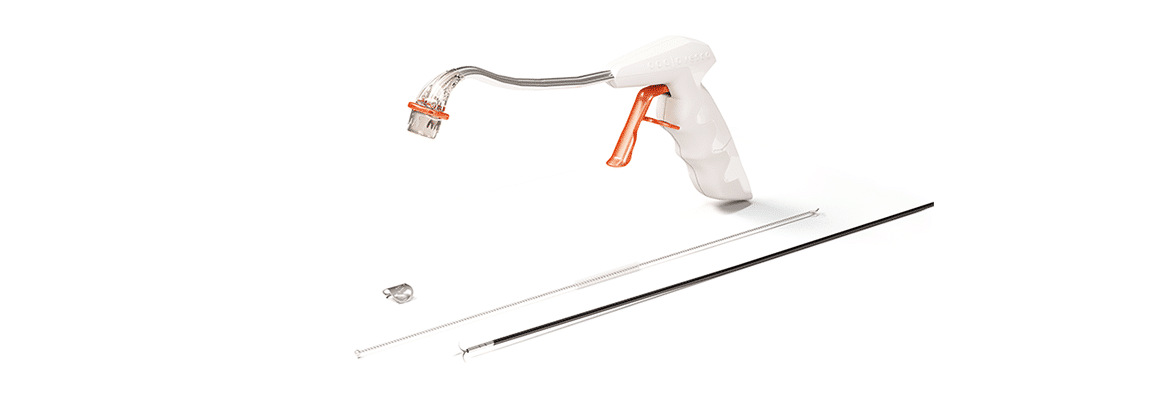
A total of 100 OTSC Proctology procedures were performed in 96 patients (median age 50 years, range 20-80 years, 64 male, 32 female) with 55 transsphincteric, 38 suprasphincteric, 2 extrasphincteric and 5 rectovaginal fistulas. All but 11 fistulas (8 Crohn’s disease, 3 ulcerative colitis) were of cryptoglandular origin. In 73 cases, the clip was used as first-line therapy, whereas in 27 cases, OTSC Proctology was applied in recurrent fistulas. Minimally invasive surgery with the OTSC Proctology was performed according to a standardized technique: the fistula tract was debrided using a special fistula brush, and the clip was applied on the internal fistula opening. The median operation time was 32 min (range 17 – 66 min). There were no major intraoperative technical problems. The transanal clip procedure was fast and easy to perform in experienced hands. In 93 % of procedures, the clip reliably closed the internal fistula opening already after the first application. Clip malplacement with inadequate fistula closure requiring clip removal and application of a new clip occurred in only 7 patients. All patients found the postoperative pain to be well controlled with standard pain medication. Patients were discharged home on the third and fourth postoperative days. 6-months follow-up data was available for 99 clip applications. On examination 6 months after surgery, 65 % of patients had no clinical signs or symptoms of their previous fistula and were considered to be healed. The healing rate for first-line fistula therapy was 79 %, whereas in recurrent fistulas, the success rate was 26 %. The healing rates of transsphincteric, suprasphincteric, extrasphincteric, and rectovaginal fistulas were 61, 74, 100, and 20 %, respectively. OTSC Proctology was successful in 45 % of fistulas associated with inflammatory bowel disease.
The authors discussed that with an overall healing rate of 65 % and a success rate of 79 % for first-line fistula treatment, the clip achieves results at least as good as established surgical techniques like the advancement flap procedure and the fistulectomy with primary sphincter reconstruction. Moreover, this is done without traumatizing the sphincter muscle and without the risk of fecal incontinence, even if surgery fails. When compared to another sphincter-preserving minimally-invasive technique, the fistula plug, which renders a maximal healing rate of 50-60 %, OTSC Proctology obviously achieves better results.
The authors concluded that the OTSC Proctology provides convincing results as first-line treatment for complex cryptoglandular fistulas. It is a safe, effective, minimally invasive, and sphincter-sparing procedure with postoperative pain comparable to other types of fistula surgery.
Short-term outcomes of a novel endoscopic clipping device for closure of the internal opening in 100 anorectal fistulas.
Prosst RL, Joos AK.
Tech Coloproctol 2016; 20:753-758.


 English
English  Français
Français