16 patients with rectovaginal fistulas, 13 of those having undergone previous surgical interventions, were treated with the OTSC Proctology. The healing rate at a median follow-up of 10.2 months was 43.7 %. Complications were pain in 4 patients and spontaneous clip detachment in 2 patients. No patients reported postoperative incontinence.
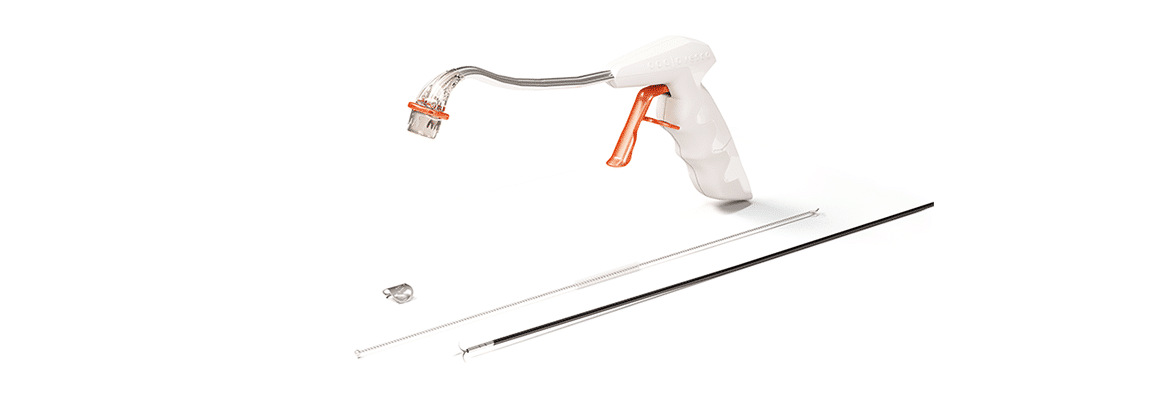
Y Tong et al., Michallon University Hospital, Grenoble, France, published a non-randomized prospective monocentric study evaluating feasibility, safety, and effectiveness of the OTSC Proctology for rectovaginal fistula repair. The OTSC Proctology is a minimally invasive technique avoiding sphincter damage, and has the advantage of maintenance of compression force on the internal fistula opening.
16 consecutive patients with a median age of 40.1 years were enrolled in the study. The causes of rectovaginal fistula were adverse events following proctectomy or pelvic radiotherapy (n = 6), obstetric trauma (n = 5), inflammatory bowel disease (n = 3), and unknown (n = 2). 13 patients had undergone previous surgical interventions before the clipping procedure, thereof 7 patients up to three surgical interventions and 6 patients more than 3 surgical interventions. The fistula tract was drained by loose setons in 6 patients and 11 patients had a temporary diverting stoma at time of the clipping procedure.
The placement of the OTSC Proctology was technically successful in all cases. Healing was defined as an absence of symptoms of leakage reported by the patient, and confirmed by clinical examination, radiological contrast control through the lower limb of the colostomy if present, and examination under general or epidural anesthesia. Successful primary healing of the fistula was observed in 7 patients (43.7 %) at 8 months and this result persisted at a median follow-up of 10.2 months (range 8 – 36 months). Short-term postoperative complications were rare: one patient reported pain due to a perianal abscess that required an immediate removal of the clip and drainage. Two cases of spontaneous clip detachment were observed at 1 month follow-up. Chronic pain and ulceration around the clip led to surgical removal of the clip in three further patients. Most recurrences appeared shortly after the procedure, with a median delay of 45 days (range 16 – 217). No patients reported postoperative incontinence.
The authors concluded that the OTSC Proctology is feasible, safe and effective for rectovaginal fistula repair. Further trials are needed, incorporating comparisons to well-established techniques, a longer follow-up period, and a larger cohort.
Short-term outcomes of the over-the-scope clip proctology system for rectovaginal fistula repair: a prospective study
Tong Y, Trilling B, Sage P, Girard E, Faucheron J.
Techniques in Coloproctology 2019; 23:245-249. https://doi.org/10.1007/s10151-019-01948-5


 English
English  Français
Français